A significant new study published in Lancet Neurology shows that over 3 billion people worldwide suffered from neurological disorders in 2021. Neurological conditions such as stroke, epilepsy, and dementia cause 9 million deaths globally each year, ranking them among the leading causes of death and disability worldwide. In 2021, the top ten neurological disorders contributing to health loss were stroke, neonatal encephalopathy (brain injury), migraine, dementia, diabetic neuropathy (nerve damage), meningitis, epilepsy, neurological complications in preterm infants, autism spectrum disorder, and nervous system cancers. At the World Health Assembly held in 2022, Member States adopted the Intersectoral Global Action Plan on Epilepsy and Other Neurological Disorders 2022–2031, providing a roadmap for countries to improve the prevention, early detection, treatment, and rehabilitation of neurological disorders.
Globally, research into the diagnosis and treatment of brain and neurological diseases continues to intensify. Consequently, brain science is one of the most prominent future research areas, holding significant importance for improving global brain health risks.
Alzheimer's Disease (AD) is a multifactorial neurodegenerative disorder and is currently the most common type of dementia-related disease. Clinical symptoms include memory impairment, intellectual decline, impaired motor coordination and balance, and in severe cases, changes in mood and personality, loss of ability for self-care, and even death. To date, there is no cure. Several hypotheses exist regarding the pathogenesis of AD, including the β-amyloid cascade hypothesis, Tau protein phosphorylation hypothesis, and cholinergic impairment hypothesis.
APP/A beta, APOE, Tau, VLDLR, ACHE, TREM2, Nogo Receptor, BCHE, BACE-1, GSK-3beta, NPTX2, NEFL, TDP43, AD7c-NTP
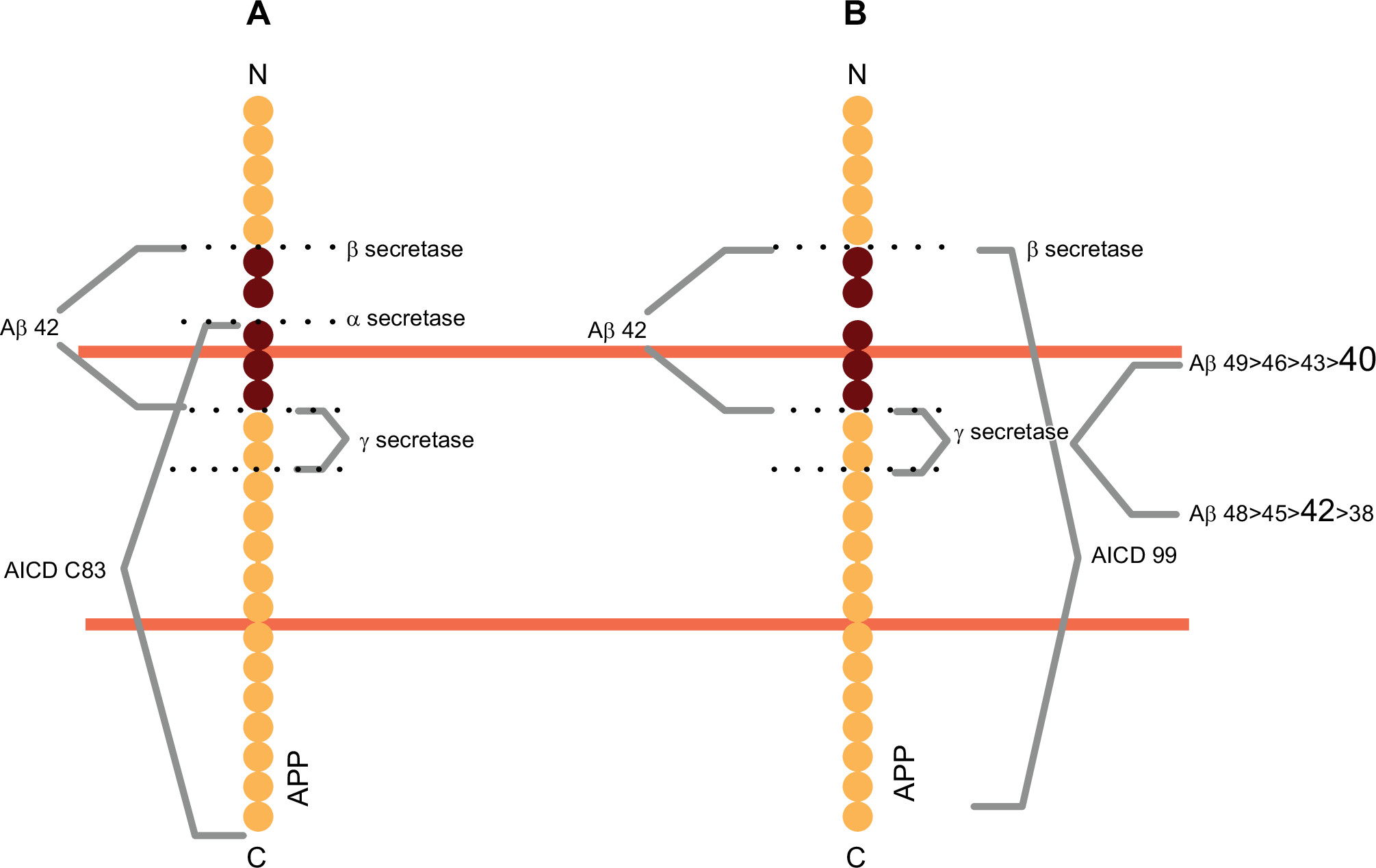
Two distinct pathways of Amyloid Precursor Protein (APP) processing
(Physiol Rev. 2021 Jul 1;101(3):1047-1081.)
Parkinson's Disease (PD) is the second most common central neurodegenerative disorder. Its primary clinical manifestations include resting tremor, muscle rigidity, bradykinesia (slowness of movement), and postural instability. The typical pathological feature is the progressive degeneration and loss of dopaminergic neurons in the substantia nigra of the midbrain, with the surviving dopaminergic neurons containing intracytoplasmic pathological inclusions called Lewy bodies. The exact cause and pathogenesis of PD are not fully understood. It is currently believed that PD likely results from the combined effects of genetic, environmental, and aging factors. Specific mechanisms involve mitochondrial dysfunction, oxidative stress, neuroinflammation, and excitotoxic damage. The average age of onset for PD is 55 years, and its incidence increases significantly with age.
SNCA/ Alpha-Synuclein, CNTFR, DDC, GFRAL, LRRK2, MAOA, MAOB,
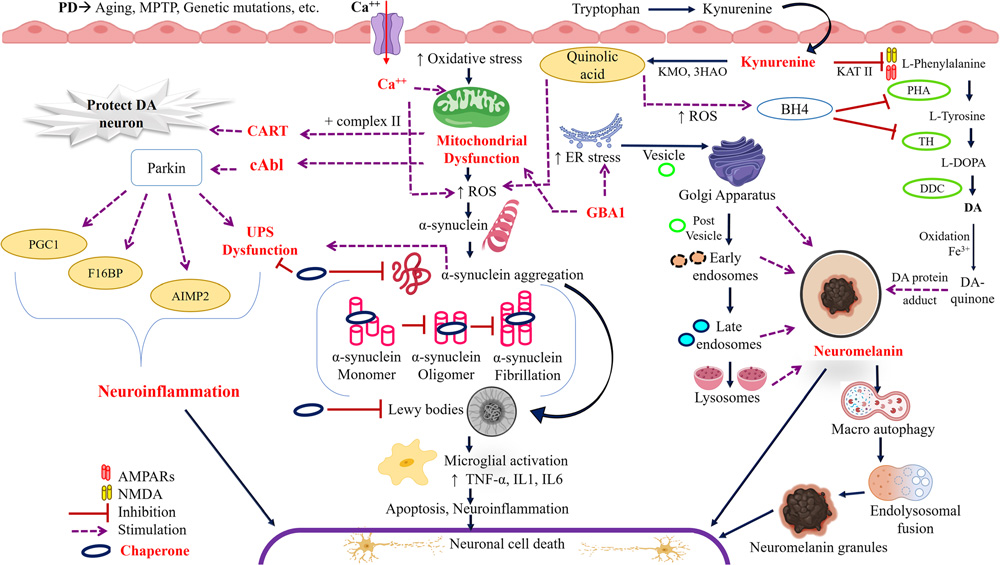
Pathogenic mechanisms of Parkinson's disease
(BIOCELL 2024, 48(8), 1155-1179)
Huntington's Disease (HD) is an autosomal dominant, progressive neurodegenerative disorder. It is caused by a CAG repeat expansion in the first exon of the HTT gene on chromosome 4, encoding mutant huntingtin protein (mHTT). Patients develop abnormalities including chorea, dystonia, incoordination, cognitive decline, and behavioral difficulties. Research indicates that HD pathogenesis involves excitotoxicity, dopaminergic imbalance, mitochondrial dysfunction, metabolic defects, disruption of protein homeostasis, transcriptional dysregulation, and neuroinflammation.
HTT
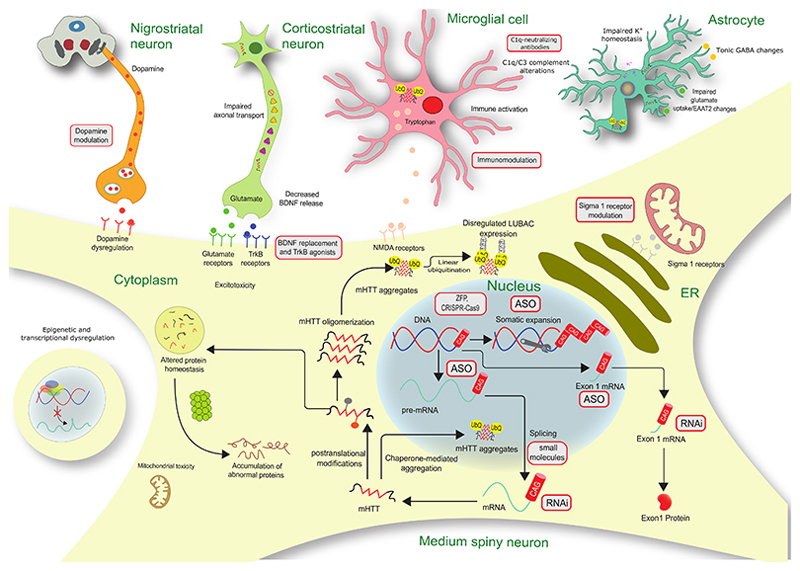
Schematic diagram of Huntington's disease pathogenesis and potential therapeutic targets
(Lancet Neurol. Author manuscript; available in PMC: 2023 Jan 1.)
Amyotrophic Lateral Sclerosis (ALS) is a neurodegenerative disorder affecting both upper and lower motor neurons, leading to muscle weakness and eventual paralysis. There is currently no cure. It is hypothesized that intra-neuronal protein aggregates associated with ALS, such as SOD1, TDP-43, and FUS, cause cellular stress and disrupt protein homeostasis by sequestering RNA and other key cellular proteins.
SOD1, TDP43
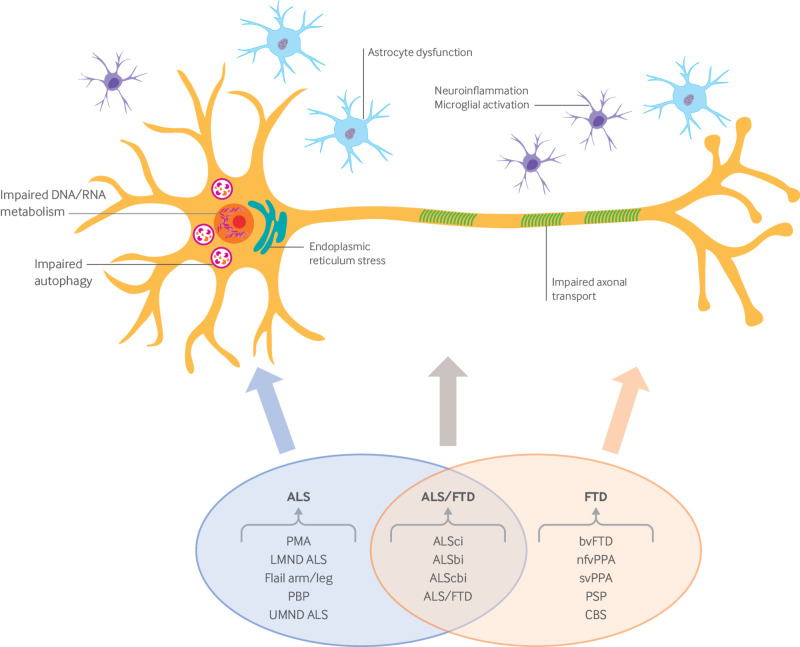
ALS clinical syndrome and disease mechanisms leading to neurodegeneration
(Am J Manag Care. 2018 Aug;24(15 Suppl):S320-S326.)
Multiple Sclerosis (MS) is an autoimmune-mediated degenerative disease of the central nervous system, characterized by disseminated, patchy demyelination within the brain and spinal cord. Common symptoms include visual and oculomotor abnormalities, sensory disturbances, weakness, spasticity, urinary dysfunction, and mild cognitive symptoms. The exact cause of MS is unknown, but Epstein-Barr virus infection, low serum vitamin D levels, insufficient sunlight exposure, and smoking have been identified as potential risk factors. B cells play a significant role in MS. Randomized clinical trials using monoclonal anti-CD20 antibodies Rituximab and Ocrelizumab to treat MS have shown significant reductions in new lesion formation and annual relapse rates.
CD20/MS4A1, CD52, GPC4
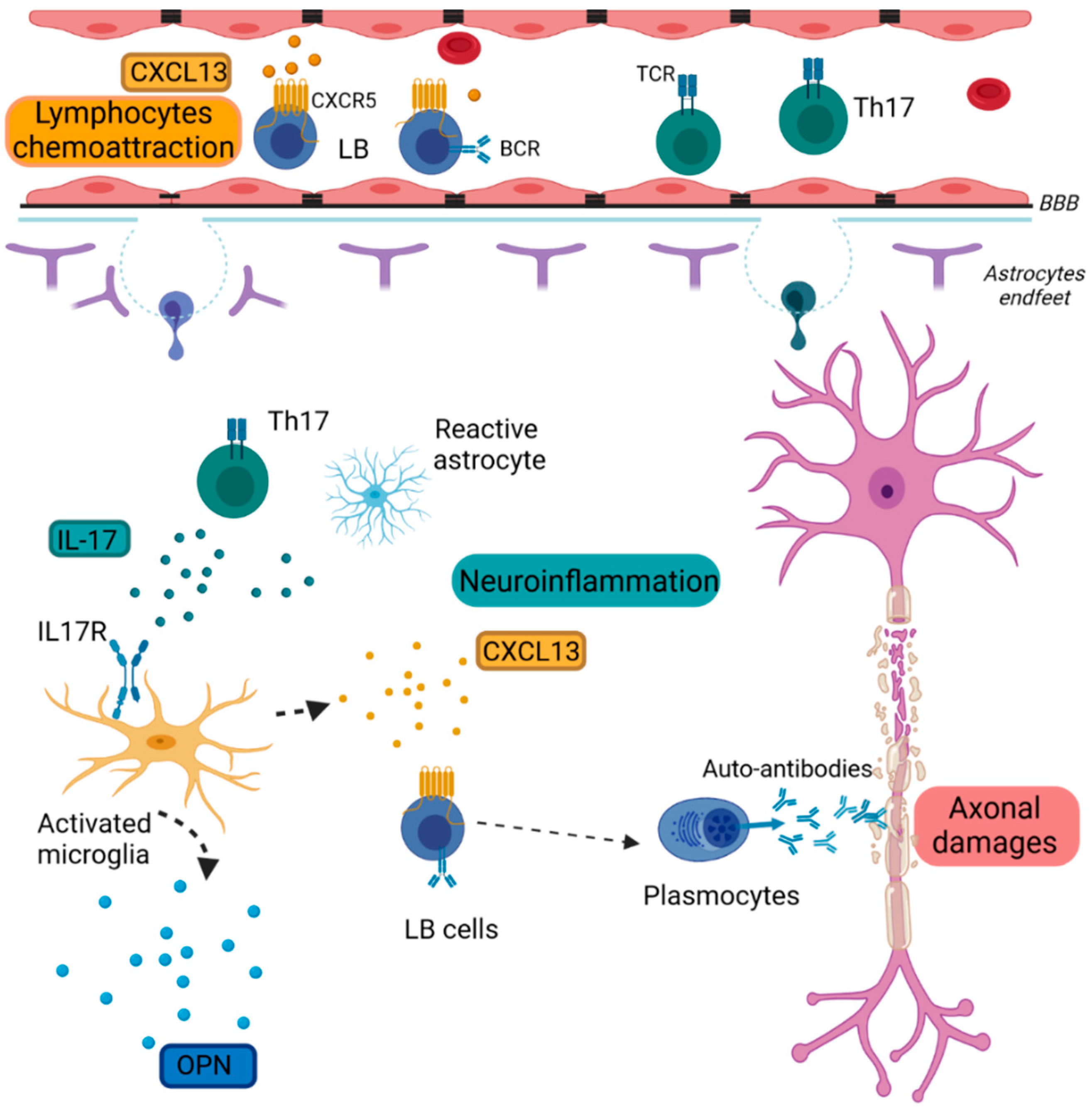
Schematic diagram of inflammation in MS pathology
(Int J Mol Sci. 2022 Sep 29;23(19):11532.)
Spinal Muscular Atrophy (SMA) is an autosomal recessive lower motor neuron disease. It involves the degeneration of nerve cells originating from the spinal cord and brainstem, primarily due to mutations in the survival motor neuron gene 1 (SMN1), leading to degeneration of alpha motor neurons in the anterior horn of the spinal cord. Severe muscle weakness and atrophy are the main clinical features. The SMN gene responsible for this condition is located on chromosome 5q11.2-13.3. Within this region, there are two highly similar SMN genes: SMN1 and SMN2. The SMN protein translated from the SMN1 gene is mostly fully functional, while the SMN2 gene produces only a very small amount of fully functional SMN protein; the functional capacity of SMN1 is approximately 10 times that of SMN2. Due to the high sequence similarity between the SMN1 and SMN2 gene blocks, deletions or conversions between these genes frequently occur. About 95% of SMA patients (including types I, II, and III) have deletions or conversions of the SMN1 gene, while the remaining 5% have intragenic mutations within the SMN1 gene. If a patient lacks both copies of the SMN1 gene, the number of SMN2 gene copies determines the severity of the disease. Type III SMA patients are more likely to have four copies of the SMN2 gene compared to type I patients. Diagnosis of SMA is primarily done through blood tests to detect the presence of the SMN1 gene, combined with physical examination and family history. There is currently no specific cure for SMA, but prenatal genetic diagnosis can prevent the birth of a fetus carrying the pathogenic gene.
SMN1, SMN2
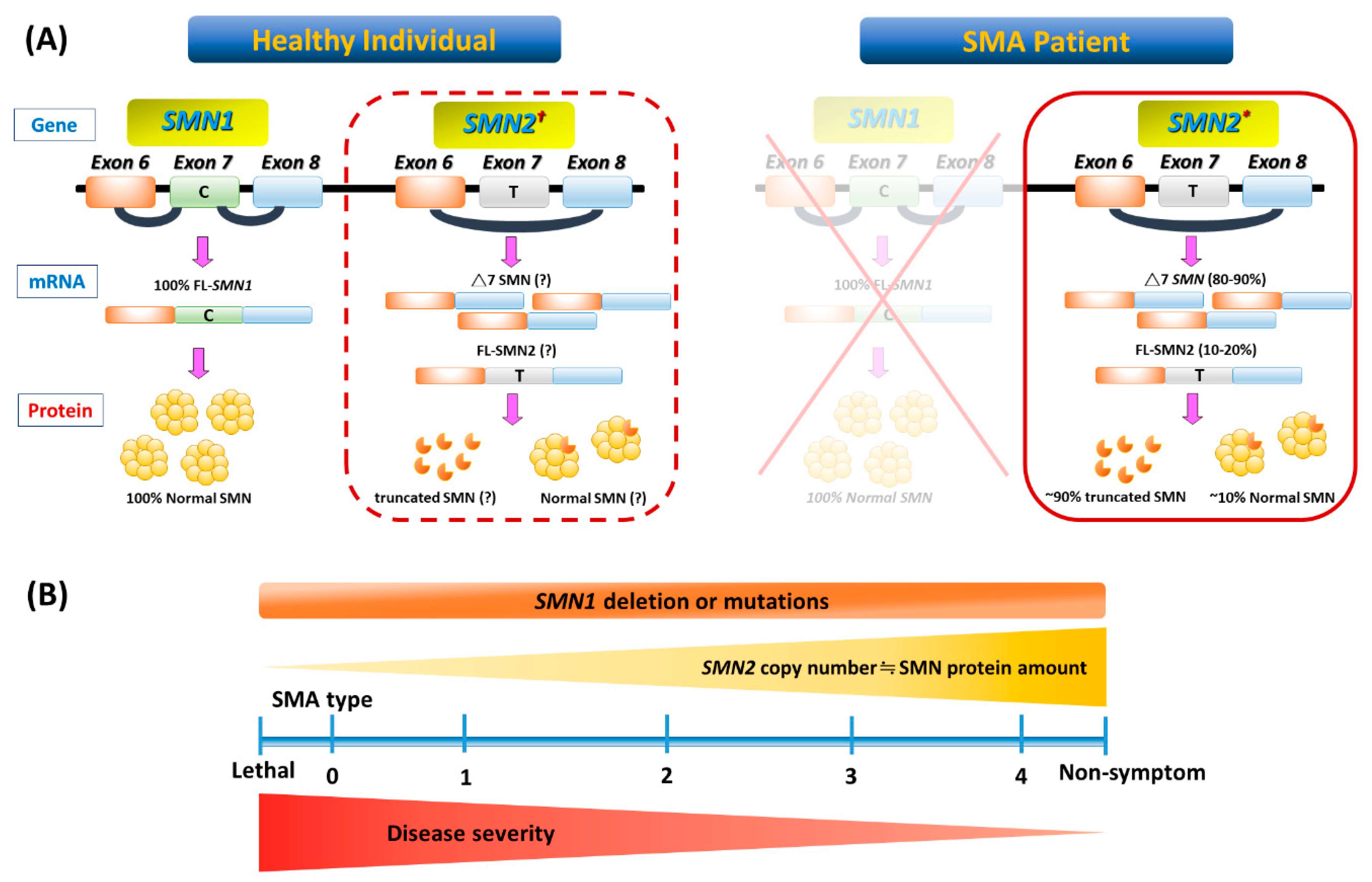
Genetic basis and phenotype-genotype correlation in SMA
(Int J Mol Sci. 2020 May 7;21(9):3297.)
The neuropsychiatric disorder spectrum encompasses a range of conditions from functional neurological disorders (such as epilepsy, Attention Deficit Hyperactivity Disorder (ADHD), Autism Spectrum Disorder (ASD)) to psychiatric illnesses (such as schizophrenia, bipolar disorder, major depressive disorder, anxiety disorders). Although clinical presentations vary, modern neuroscience research reveals that these disorders share complex neurobiological underpinnings, involving interactions between genetic susceptibility and environmental factors. Psychiatric illnesses, once primarily considered "functional" or "psychological," are now clearly associated with detectable pathological changes in the central nervous system. These include abnormal neural circuit function, dysregulation of neurotransmitter systems, and characteristic changes observed at the molecular and cellular levels.
CNTN2/TAG1, NRGN, NPTX2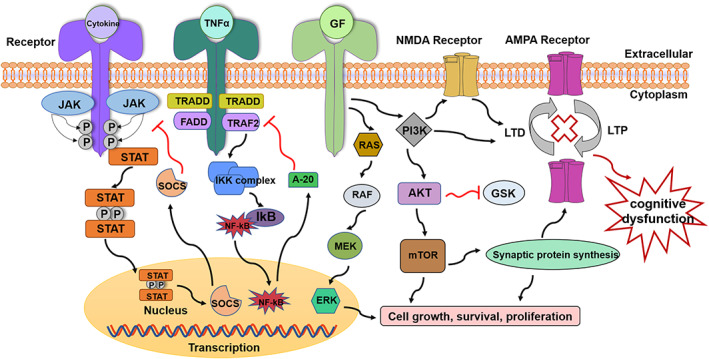
Three most common cytokine pathways implicated in cognitive dysfunction
(Cell Prolif. 2022 Jul 20;55(10):e13295.)
AntibodySystem, as a professional protein and antibody supplier, offers a series of high-quality proteins and antibodies related to brain and neurological disease research, advancing global brain health research progress. Explore more neuroscience research tools here.